AI Post-Enrollment Audit Agent
Automating Post-Enrollment Audit with AI
Verify dependent eligibility against plan rules automatically
The agent validates submitted documentation—marriage certificates, birth certificates, court orders—against your SPD definitions and carrier requirements, flagging ineligible dependents and timing violations without manual review.
Reconcile enrollment data with carrier invoices and payroll
AI automation surfaces discrepancies between your HRIS, carrier rosters, and billing data—identifying enrollment-only exceptions, carrier-bill-only items, tier mismatches, and effective date misalignments in a single pass.
Generate corrected feeds and compliance documentation
Automated workflows produce updated 834 enrollment files, payroll adjustment reports, COBRA notifications, and audit trail artifacts ready for ERISA fiduciary attestation.
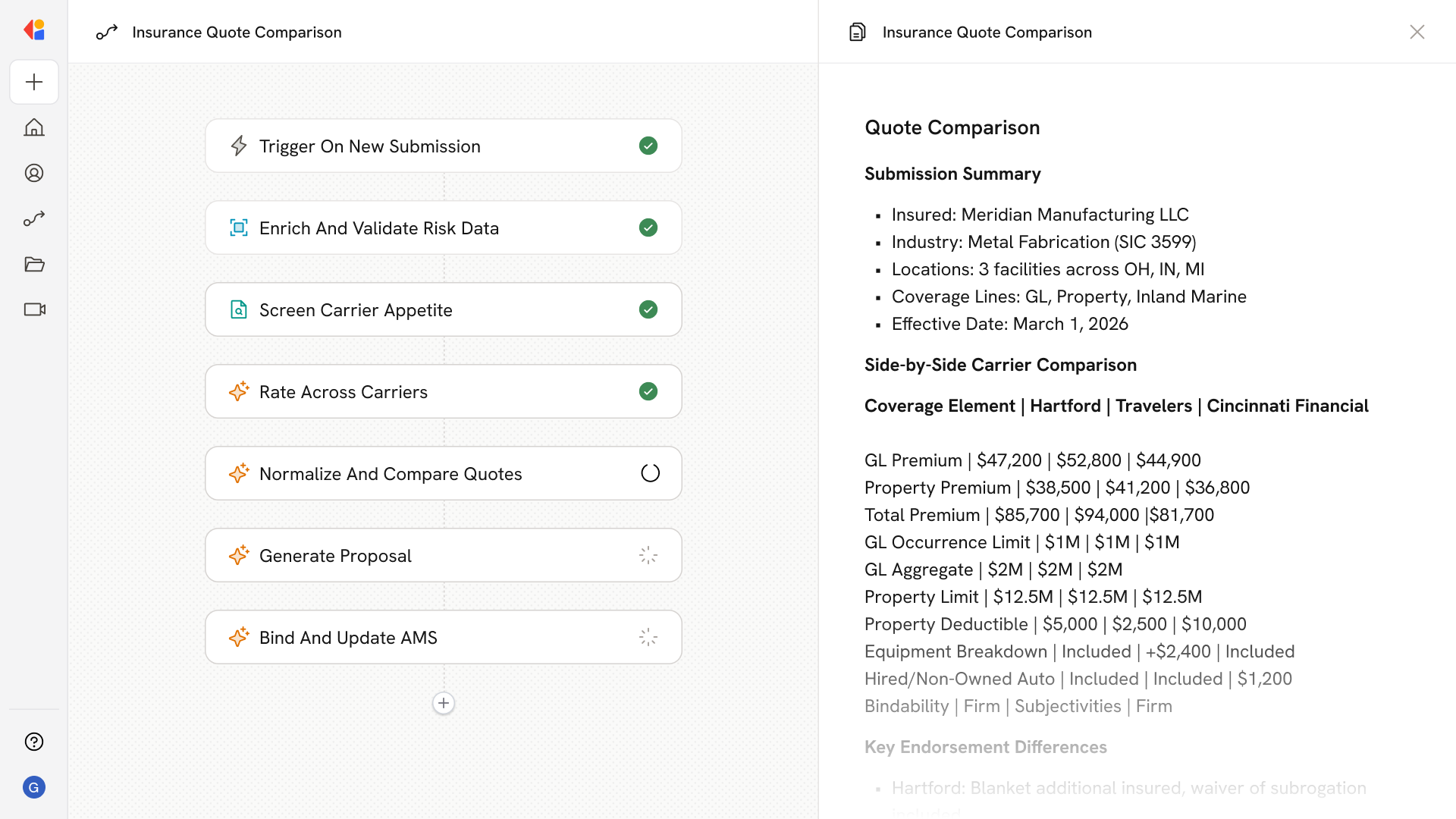
How Cassidy automates post-enrollment audit using AI
Step 1: Ingest enrollment and carrier data
The Workflow triggers after open enrollment closes, pulling eligibility census data from your HRIS, OE election snapshots, carrier invoices, and payroll deduction files into Cassidy's Knowledge Base for unified analysis.
Step 2: Validate dependent documentation
Cassidy reviews submitted documents—marriage certificates, birth certificates, adoption decrees, domestic partner affidavits—against your plan's eligibility rules, checking date alignment, age limits, and dependent class requirements.
Step 3: Flag exceptions and eligibility mismatches
The agent generates an exception inventory categorizing missing documentation, invalid proofs, aged-out dependents, ex-spouse coverage, and timing violations, with each issue tagged by severity and required action.
Step 4: Reconcile enrollment against carrier and payroll records
Cassidy cross-references your enrollment data with carrier rosters and billing files, identifying discrepancies: enrollment-only items, carrier-bill-only charges, rate mismatches, tier errors, and effective date misalignments.
Step 5: Generate corrected files and audit reports
The Workflow produces updated EDI 834 enrollment feeds, payroll adjustment summaries, COBRA notifications for disenrolled dependents, and a comprehensive audit report showing ineligible dependent rates, premium leakage avoided, and remediation actions.
Step 6: Route for Human-in-the-Loop review
Complex cases—appeals, QMCSO orders, state mandate exceptions—are routed to your benefits team with full context and recommended actions, keeping you in control of final decisions.
Implement it inside your company
- Hands-on onboarding and support
- Self-paced training for your team
- Dedicated implementation experts
- Ongoing use case discovery
- ROI tracking & analytics dashboards
- Proven playbooks to get started fast